This is new evidence that diet plays a central role in irritable bowel syndrome (or “functional colopathy”). A study recently published in the journal The Lancet Gastroenterology
To reach this conclusion, researchers at the University of Gothenburg, in Sweden, tested three types of treatments on 300 patients for a month. A first group had to follow a diet low in Fodmaps, that is to say excluding foods containing sugars that are poorly absorbed in the intestine. We can cite lactose, contained in dairy products; fructans, which are found in wheat, rye and barley; fructose, present in fruits, but also added to all industrially prepared meals; or even galactans, which are mainly found in legumes (chickpeas, lentils, etc.).
A second group followed a “Low carb” diet, low in carbohydrates but high in protein. The patients in the third group were, for their part, treated with antispasmodic, laxative or antidiarrheal drugs. After one month of treatment, all three groups saw their symptoms and quality of life improve. But not in the same proportions: three-quarters of patients who followed one of the two diets saw their condition improve, compared to “only” half of the people treated with medication.
The benefits of the diets were even felt over time, since, six months later, the majority of participants were doing well even though they had gradually returned to their usual diet. “This finding indicates that small reductions in Fodmaps and carbohydrate intake could have beneficial effects,” emphasize the authors of the study.
In practice, the low-Fodmap diet is already recommended to treat irritable bowel syndrome, but not the “Low carb” diet, rich in protein, for which evidence of effectiveness is lacking. “The low Fodmaps diet consists of temporarily eliminating all foods containing fermentable sugars because these increase the secretion of water in the small intestine, which generates bloating, and they ferment in the colon, which generates gas,” explains Professor Benoît Coffin, head of the hepato-gastroenterology department at Louis-Mourier hospital, in Colombes (Hauts-de-Seine). Retained water and gases cause distension of the digestive tract, causing pain.
“Many patients think that they are intolerant or allergic to this or that food, in particular to gluten, but this is not the case,” explains Professor François Mion, head of the functional digestive exploration department at the Édouard-Herriot hospital, in Lyon. “Irritable bowel syndrome results from hypersensitivity of the gut-brain axis and fermentable sugars accentuate this phenomenon,” he continues.
On paper, the idea is simple: completely remove Fodmaps sources for six to eight weeks. “If the patient is better, we ask him to gradually reintroduce the different families of foods so that he can determine that they are the acceptable doses for him,” indicates Professor François Mion. The first effects generally begin to be felt after one to two weeks. But in reality, eliminating these sugars from our diet is a big challenge. “It’s a difficult diet to follow because a lot of foods contain it: a lot of fruits and vegetables, all products derived from wheat, industrial dishes…”, lists the gastroenterologist.
Fortunately, there are alternatives. Rather than milk and yogurts, you should, for example, turn to lactose-free milk, plant-based drinks (soy, oats, etc.) or even soy yogurts. On the fruit side, apples, pears, peaches or even apricots must give way to bananas, pineapple, citrus fruits or even melon. “We must also eliminate all foods made from wheat, barley and rye because these contain a type of starch that is resistant to digestion,” specifies Professor Benoît Coffin. Goodbye, therefore, pasta, semolina, flour, bread, cereals. “Buckwheat, spelt, rice or oats, in all their forms, can replace wheat-based products,” argues Professor Mion.
“It’s a diet that works well and is prescribed very often, it’s worth trying,” encourages Professor Coffin, while recognizing the constraints that this represents. Moreover, going without all these fermentable carbohydrates can lead to an unbalanced diet and cause deficiencies. The ideal is therefore to seek help from a nutritionist doctor or a dietitian, especially if you are prone to eating disorders.
“It’s not easy, because you have to find a professional who knows this disease well and you have to have sufficient income to afford this care because it is not covered,” underlines Professor François Mion. In several cities (Lyon, Paris, Rouen, Nancy, Bordeaux, etc.), hospitals have however set up reimbursed care pathways, where it is possible to do everything at once: medical consultation, dietetic sessions and support. psychological burden. But you have to be patient. “In our hospital, the waiting time is three to four months,” explains Professor Mion.
 Gaza: under the spotlight, the Israeli-Palestinian conflict shakes up the Eurovision contest
Gaza: under the spotlight, the Israeli-Palestinian conflict shakes up the Eurovision contest Black soldier killed by a police officer in the United States: the sheriff publishes the video of the arrest
Black soldier killed by a police officer in the United States: the sheriff publishes the video of the arrest In Malmö, the Eurovision party transformed into entrenched camps
In Malmö, the Eurovision party transformed into entrenched camps In Russia, Vladimir Putin stigmatizes “Western elites”
In Russia, Vladimir Putin stigmatizes “Western elites” “Mediterranean diet” or “DASH”, two good tips for eating better
“Mediterranean diet” or “DASH”, two good tips for eating better Fatal case of cholera in Mayotte: the epidemic is “contained”, assures the government
Fatal case of cholera in Mayotte: the epidemic is “contained”, assures the government The presence of blood in the urine, a warning sign of bladder cancer
The presence of blood in the urine, a warning sign of bladder cancer A baby whose mother smoked during pregnancy will age more quickly
A baby whose mother smoked during pregnancy will age more quickly Artificial intelligence lies, cheats and deceives us, and that's a problem, experts warn
Artificial intelligence lies, cheats and deceives us, and that's a problem, experts warn Google Cloud mistakenly deletes UniSuper fund account and deprives 600,000 Australians of their superannuation
Google Cloud mistakenly deletes UniSuper fund account and deprives 600,000 Australians of their superannuation IBM, Amazon, Hager... These record investments expected at the Choose France summit
IBM, Amazon, Hager... These record investments expected at the Choose France summit Boeing's black streak: a second Air France flight diverted in three days for “a smell of heat”
Boeing's black streak: a second Air France flight diverted in three days for “a smell of heat” Eurovision 2024: Bernard-Henri Lévy will vote for the “courageous” Eden Golan in the face of “the wind of hatred against the Jews”
Eurovision 2024: Bernard-Henri Lévy will vote for the “courageous” Eden Golan in the face of “the wind of hatred against the Jews” Eurovision 2024: Joost Klein, the Dutch candidate, excluded from the competition
Eurovision 2024: Joost Klein, the Dutch candidate, excluded from the competition The origin of the vandalized world, the Musée d’Orsay files a complaint
The origin of the vandalized world, the Musée d’Orsay files a complaint London: two octogenarians charged after damaging the “Magna Carta” window
London: two octogenarians charged after damaging the “Magna Carta” window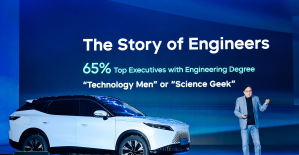 Omoda 7, another Chinese car that could be manufactured in Spain
Omoda 7, another Chinese car that could be manufactured in Spain BYD chooses CA Auto Bank as financial partner in Spain
BYD chooses CA Auto Bank as financial partner in Spain Tesla and Baidu sign key agreement to boost development of autonomous driving
Tesla and Baidu sign key agreement to boost development of autonomous driving Skoda Kodiaq 2024: a 'beast' plug-in hybrid SUV
Skoda Kodiaq 2024: a 'beast' plug-in hybrid SUV The home mortgage firm rises 3.8% in February and the average interest moderates to 3.33%
The home mortgage firm rises 3.8% in February and the average interest moderates to 3.33%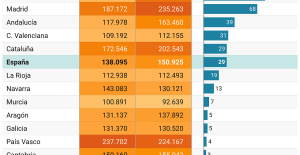 This is how housing prices have changed in Spain in the last decade
This is how housing prices have changed in Spain in the last decade The home mortgage firm drops 10% in January and interest soars to 3.46%
The home mortgage firm drops 10% in January and interest soars to 3.46% The jewel of the Rocío de Nagüeles urbanization: a dream villa in Marbella
The jewel of the Rocío de Nagüeles urbanization: a dream villa in Marbella Diving into the secrets of the National Assembly
Diving into the secrets of the National Assembly Institutions: senators want to restore the accumulation of mandates and put an end to the automatic presence of ex-presidents on the Constitutional Council
Institutions: senators want to restore the accumulation of mandates and put an end to the automatic presence of ex-presidents on the Constitutional Council Europeans: David Lisnard expresses his “essential and vital” support for François-Xavier Bellamy
Europeans: David Lisnard expresses his “essential and vital” support for François-Xavier Bellamy Facing Jordan Bardella, the popularity match turns to Gabriel Attal’s advantage
Facing Jordan Bardella, the popularity match turns to Gabriel Attal’s advantage These French cities that will boycott the World Cup in Qatar
These French cities that will boycott the World Cup in Qatar Top 14: in video, the incredible 100 meter test scored by Aviron Bayonnais against Racing
Top 14: in video, the incredible 100 meter test scored by Aviron Bayonnais against Racing Top 14: A Graou-Mallia hinge, Capuozzo back... the composition of Stade Toulousain for the classico.
Top 14: A Graou-Mallia hinge, Capuozzo back... the composition of Stade Toulousain for the classico. MotoGP: It won't be easy for Bagnaia to win a third title, says legend Valentino Rossi
MotoGP: It won't be easy for Bagnaia to win a third title, says legend Valentino Rossi Handball: the Blues win easily against the United States
Handball: the Blues win easily against the United States