As a result of the pandemic rule, coverage for as many as 15,000,000 people could be lost.
Prior to the crisis, U.S. States regularly checked Medicaid recipients' eligibility to ensure they were still eligible for coverage. This was based on income and residency. This is usually 138% of the federal poverty level. The state-specific rates vary. To qualify, one California person cannot earn more than $17 609 per year.
However, during the pandemic, a provision of the Families First Coronavirus Response Act put a pause button on eligibility status checks. This ensured that recipients received continuous Medicaid coverage during the crisis. Many signed up for Medicaid coverage after losing their jobs, and often their insurance. This helped to increase the number of beneficiaries in the program to 76.7 million as of July 2021 (the latest data available). That's a 19% increase since 2019.
According to Matthew Buettgens (senior fellow at Urban Institute), the pause in the eligibility status check process will end in April. This could mean that as many as 15,000,000 people may be thrown off Medicaid. This is a complicated issue because low-income individuals may lose coverage by not providing income verification.
Buettgens stated that states are processing an unprecedented amount of participants in a very short timeframe. "There are concerns that this could lead more people to be unenrolled than they need, even though they may still be eligible."
Telephone wait time of two hours
Many health care advocates worry about how states will handle eligibility checks for record numbers of enrollees. This is despite the fact that agency staffing levels are low due to a national labor shortage or budget cuts. Texas, for example, added 1 million Medicaid beneficiaries during the pandemic. However, its Medicaid division has been reduced by the Houston Chronicle.
"We are concerned that a lot people don't know they must enroll. If they do, how quickly will the state process them? Jana Eubank is the executive director of Texas Association of Community Health Centers.
She also noted that updating one's eligibility requirements can take time for Medicaid recipients. Eubank said that enrollees who have not logged in to the online system to update their information might have forgotten their password. However, the Texas system does not allow for the recovery of forgotten passwords electronically.
"To reset your password, you must call 211. In some cases, we hear from patients that they have to wait up to two hours," she said, referring to the Texas social service hotline.
"Unprecedented situation"
Prior to the pandemic, Medicaid enrollment had been falling. The Kaiser Family Foundation reported that the number of Medicaid enrollees fell by 3% between December 2017 and December 2019. The analysis revealed that this was partly due to the U.S.'s growing economy over the period.
However, this trend was reversed by the pandemic. The pandemic caused the economy to collapse and millions lost their jobs. In response, lawmakers added a provision in the Families First Coronavirus Response Act. This allowed states to receive more Medicaid funding.
Medicaid enrollment has been increasing for decades, despite the drop in enrollment prior to the pandemic. In 2000, 34.5 million people were enrolled. This is less than half the current enrollment , according to the Medicaid and CHIP Payment and Access Commission. The program's spending has increased, with its outlays increasing by more than three times from $206 billion in 2020 to $683 billion in 2020.
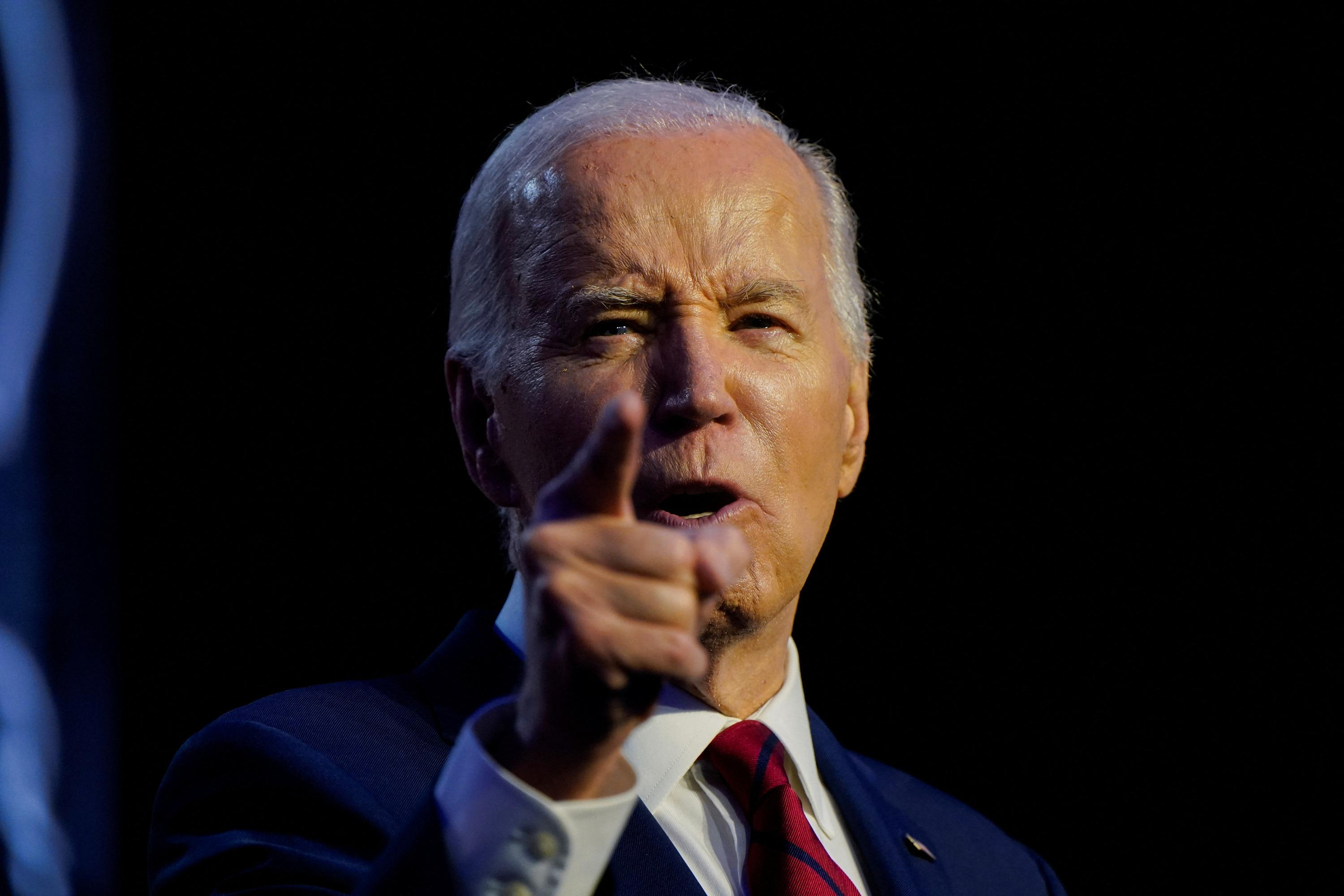
The Biden administration extended for a period of 90 days in January to reflect its conclusion that the U.S. is facing a public health emergency. Mid-April will see the end of sweeping Medicaid relief if there is no extension. This means that states will have to resume eligibility status checks despite the increase in recipients.
Buettgens stated that states "are going have to determine eligibility for an increased population than they've ever had" and could do so very quickly.
Another question is: What will happen to 15 million people who could lose coverage this year, if eligibility checks resume? Buettgens analysis showed that only about one third of those who are eligible for Affordable Care Act's subsidized private healthcare will be able to do so. Nearly all the rest will likely receive health care through their employers, given the improved labor market and increased benefits offered by employers to recruit workers.
The analysis showed that these families will have to pay higher premiums and more out-of-pocket expenses for their health insurance. Experts said that there are risks for these households to choose not to have health insurance coverage due to the higher costs or to fall through the cracks because they failed to check their eligibility status.
Buettgens stated that if people do not enroll in other forms of coverage, either because they aren't sure what they're eligible for, or because it is too expensive, this could result in an increase in the number of uninsured. It is an unprecedented situation, there is much uncertainty.
 Hamas-Israel war: US begins construction of pier in Gaza
Hamas-Israel war: US begins construction of pier in Gaza Israel prepares to attack Rafah
Israel prepares to attack Rafah Indifference in European capitals, after Emmanuel Macron's speech at the Sorbonne
Indifference in European capitals, after Emmanuel Macron's speech at the Sorbonne Spain: what is Manos Limpias, the pseudo-union which denounced the wife of Pedro Sánchez?
Spain: what is Manos Limpias, the pseudo-union which denounced the wife of Pedro Sánchez?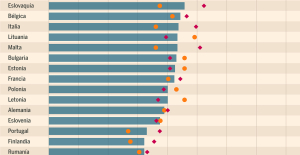 Spain is the country in the European Union with the most overqualified workers for their jobs
Spain is the country in the European Union with the most overqualified workers for their jobs Parvovirus alert, the “fifth disease” of children which has already caused the death of five babies in 2024
Parvovirus alert, the “fifth disease” of children which has already caused the death of five babies in 2024 Colorectal cancer: what to watch out for in those under 50
Colorectal cancer: what to watch out for in those under 50 H5N1 virus: traces detected in pasteurized milk in the United States
H5N1 virus: traces detected in pasteurized milk in the United States Private clinics announce a strike with “total suspension” of their activities, including emergencies, from June 3 to 5
Private clinics announce a strike with “total suspension” of their activities, including emergencies, from June 3 to 5 The Lagardère group wants to accentuate “synergies” with Vivendi, its new owner
The Lagardère group wants to accentuate “synergies” with Vivendi, its new owner The iconic tennis video game “Top Spin” returns after 13 years of absence
The iconic tennis video game “Top Spin” returns after 13 years of absence Three Stellantis automobile factories shut down due to supplier strike
Three Stellantis automobile factories shut down due to supplier strike A pre-Roman necropolis discovered in Italy during archaeological excavations
A pre-Roman necropolis discovered in Italy during archaeological excavations Searches in Guadeloupe for an investigation into the memorial dedicated to the history of slavery
Searches in Guadeloupe for an investigation into the memorial dedicated to the history of slavery Aya Nakamura in Olympic form a few hours before the Flames ceremony
Aya Nakamura in Olympic form a few hours before the Flames ceremony Psychiatrist Raphaël Gaillard elected to the French Academy
Psychiatrist Raphaël Gaillard elected to the French Academy Skoda Kodiaq 2024: a 'beast' plug-in hybrid SUV
Skoda Kodiaq 2024: a 'beast' plug-in hybrid SUV Tesla launches a new Model Y with 600 km of autonomy at a "more accessible price"
Tesla launches a new Model Y with 600 km of autonomy at a "more accessible price" The 10 best-selling cars in March 2024 in Spain: sales fall due to Easter
The 10 best-selling cars in March 2024 in Spain: sales fall due to Easter A private jet company buys more than 100 flying cars
A private jet company buys more than 100 flying cars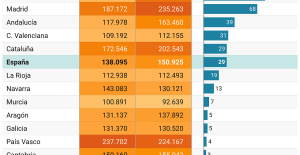 This is how housing prices have changed in Spain in the last decade
This is how housing prices have changed in Spain in the last decade The home mortgage firm drops 10% in January and interest soars to 3.46%
The home mortgage firm drops 10% in January and interest soars to 3.46% The jewel of the Rocío de Nagüeles urbanization: a dream villa in Marbella
The jewel of the Rocío de Nagüeles urbanization: a dream villa in Marbella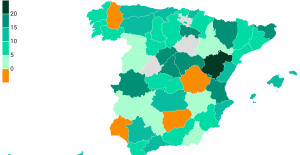 Rental prices grow by 7.3% in February: where does it go up and where does it go down?
Rental prices grow by 7.3% in February: where does it go up and where does it go down? “Deadly Europe”, “economic decline”, immigration… What to remember from Emmanuel Macron’s speech at the Sorbonne
“Deadly Europe”, “economic decline”, immigration… What to remember from Emmanuel Macron’s speech at the Sorbonne Sale of Biogaran: The Republicans write to Emmanuel Macron
Sale of Biogaran: The Republicans write to Emmanuel Macron Europeans: “All those who claim that we don’t need Europe are liars”, criticizes Bayrou
Europeans: “All those who claim that we don’t need Europe are liars”, criticizes Bayrou With the promise of a “real burst of authority”, Gabriel Attal provokes the ire of the opposition
With the promise of a “real burst of authority”, Gabriel Attal provokes the ire of the opposition These French cities that will boycott the World Cup in Qatar
These French cities that will boycott the World Cup in Qatar Judo: Blandine Pont European vice-champion
Judo: Blandine Pont European vice-champion Swimming: World Anti-Doping Agency appoints independent prosecutor in Chinese doping case
Swimming: World Anti-Doping Agency appoints independent prosecutor in Chinese doping case Water polo: everything you need to know about this sport
Water polo: everything you need to know about this sport Judo: Cédric Revol on the 3rd step of the European podium
Judo: Cédric Revol on the 3rd step of the European podium