Since 1990, the prevalence of lung cancer has practically doubled in France. Each year, it is detected in 50,000 new patients, with a clear increase in its incidence in women (4% per year according to the National Cancer Institute). This cancer is still responsible for more than 33,000 deaths per year. A gloomy outlook often attributable to too late diagnosis: it is estimated that the 5-year survival of lung cancers detected at an advanced stage is around 15%. Early detection therefore represents an important issue, because it allows curative treatments to be implemented early, which increase the chances of survival.
Over the last two decades, numerous studies have demonstrated the effectiveness of low-dose chest CT (or low-dose CT) for monitoring lung cancers. This technique produces detailed images of the thorax, and has the advantage of detecting nodules of a few millimeters, invisible on a simple chest x-ray, while using a reduced quantity of radiation. American and European learned societies have validated the use of this technique to screen populations at risk (smokers or ex-smokers aged 55 to 74). The latest study, published in November 2023 in Radiology, reveals that this method would considerably increase the survival rate 20 years after screening. However, despite the growing evidence in favor of its use, low-dose CT is still not systematically implemented in France. “An alarming finding,” underlines Gérard Zalcman, head of the thoracic oncology department at Bichat hospital (AP-HP).
» READ ALSO - Lung cancer: the idea of screening is gaining ground
Historically, the NLST studies, in the United States, and Nelson, in Europe, were the first to demonstrate the benefit of low-dose CT screening on the survival of at-risk patients: the first, in 2011, showed that this technique would reduce the mortality rate of those screened by 20% compared to subjects who were only subjected to a chest x-ray. In the Nelson study (2018), this rate was lowered by 26% among men and 40% among women.
Another study published in mid-November as part of the I-ELCAP program (the international action program against early lung cancer) found a survival rate of 81%, with a 20-year follow-up, in 1,257 subjects diagnosed at an early stage by low-dose CT. The researchers' first estimates in 2006 already indicated a 10-year survival rate of 80%, “which demonstrates the long-term impact on survival even after 20 years of follow-up,” explains Professor Zalcman. However, “this rate is probably overestimated,” underlines Marie-Pierre Revel-Dubois, radiologist at the University Hospitals of Paris (AP-HP) and responsible for screening for the French Society of Radiology. “As indicated in the study, only 44% of the 1257 subjects with cancer had a follow-up of more than 10 years, or barely half. Despite this, the study presents the longest follow-up and remains reassuring.
In view of the growing evidence, “systematic screening for lung cancer using low-dose CT should be offered to all patients at risk, smokers or ex-smokers who have quit, and supported by National Solidarity,” insists the Dr. Zalcman. However, in France, this is not yet the case, as the members of the “Together we lungs” collective pointed out during the “Novembre Perle” operation last November.
At the European level, the implementation of organized lung cancer screening is only effective in Croatia and England, illustrating the difficulty of moving to real-life implementation. In December 2022, the European Council, however, encouraged all member states to launch pilot programs. For the moment, in France, “cancerous nodules are identified when the cancer is already at an advanced stage and therefore inaccessible to curative treatments. One of the problems remains that chest x-ray is ineffective for detecting lung cancer, since it does not allow lesions to be detected at the earliest stages, when they do not cause any symptoms,” recalls Gérard Zalcman.
» READ ALSO - A promising treatment against advanced lung cancer
In 2016, the HAS was against the implementation of lung cancer screening, considering its benefits “uncertain”. In addition to the financial cost of its implementation, the health authority raised that “the reduction in mortality thanks to this screening has not been established in the French context” and that this method generated too many false positives, with patients diagnosed wrongly of a cancer that actually does not exist. “However, if it is true that the NLST test was accompanied by a high rate of false positives, around 18%, the authors of the Nelson study studied the increase in the volume of the nodule detected after 3 months: only the nodules that had grown were considered true positives, which made it possible to lower the false positive rate to only 2%,” emphasizes Dr. Zalcman. As for the need for evidence on the feasibility of organized screening in France, it was documented by a study conducted in 2019 under the direction of Olivier Leleu, head of the pulmonology department at the Abbeville hospital center. The study found the same results as those of the Nelson trial.
Revising its opinion, the HAS finally encouraged the National Cancer Institute (Inca), in February 2022, to promote experiments with organized lung cancer screening programs. The objective is to evaluate the feasibility of such screening in order to consider its large-scale deployment by 2030. Among other ongoing experiments, the Cascade study aims to document the relevance of chest scanning to of 2400 women at risk. “With the delayed effects of female smoking since the 1970s, cases of lung cancer increased from 16% in 2000 to 34% in 2020 according to statistics from general hospitals. It is therefore urgent to take an interest in this population which is increasingly affected by this pathology,” insists Dr Revel-Dubois.
In the meantime, specialists emphasize the importance of combining screening with personalized smoking cessation support programs. “Screening can significantly increase the chances of survival. But in no case will it solve the problem at its root. For this it is important to encourage a change of life towards a tobacco-free future,” recalls the radiologist.
 Body warns BBVA that "the Government has the last word" in the takeover bid for Sabadell
Body warns BBVA that "the Government has the last word" in the takeover bid for Sabadell Finding yourself face to face with a man or a bear? The debate that shakes up social networks
Finding yourself face to face with a man or a bear? The debate that shakes up social networks Sabadell rejects the merger with BBVA and will fight to remain alone
Sabadell rejects the merger with BBVA and will fight to remain alone In Germany, the far left wants to cap the price of “doner kebabs”
In Germany, the far left wants to cap the price of “doner kebabs” The presence of blood in the urine, a warning sign of bladder cancer
The presence of blood in the urine, a warning sign of bladder cancer A baby whose mother smoked during pregnancy will age more quickly
A baby whose mother smoked during pregnancy will age more quickly The euro zone economy grows in April at its best pace in almost a year but inflationary pressure increases
The euro zone economy grows in April at its best pace in almost a year but inflationary pressure increases Children born thanks to PMA do not have more cancers than others
Children born thanks to PMA do not have more cancers than others Argentina: the street once again raises its voice against President Javier Milei
Argentina: the street once again raises its voice against President Javier Milei Spain: BBVA bank announces a hostile takeover bid for its competitor Sabadell
Spain: BBVA bank announces a hostile takeover bid for its competitor Sabadell New black series for Boeing: eleven injured after a plane went off the runway in Dakar
New black series for Boeing: eleven injured after a plane went off the runway in Dakar “The prices are astronomical”: to enjoy the Olympics with family, Sabrina spent... 8,000 euros
“The prices are astronomical”: to enjoy the Olympics with family, Sabrina spent... 8,000 euros Berry affair: Jeane Manson victim of a heart problem after a court hearing
Berry affair: Jeane Manson victim of a heart problem after a court hearing Venice Film Festival: Isabelle Huppert will chair the jury of the 81st festival
Venice Film Festival: Isabelle Huppert will chair the jury of the 81st festival Louvre: Delacroix’s “Liberty Leading the People” target of the Riposte Alimentaire collective
Louvre: Delacroix’s “Liberty Leading the People” target of the Riposte Alimentaire collective The Coubertin Spirit, Eternal Memory, Planet of the Apes... Films to watch this week
The Coubertin Spirit, Eternal Memory, Planet of the Apes... Films to watch this week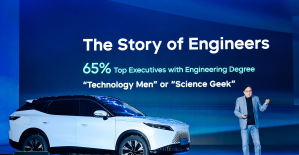 Omoda 7, another Chinese car that could be manufactured in Spain
Omoda 7, another Chinese car that could be manufactured in Spain BYD chooses CA Auto Bank as financial partner in Spain
BYD chooses CA Auto Bank as financial partner in Spain Tesla and Baidu sign key agreement to boost development of autonomous driving
Tesla and Baidu sign key agreement to boost development of autonomous driving Skoda Kodiaq 2024: a 'beast' plug-in hybrid SUV
Skoda Kodiaq 2024: a 'beast' plug-in hybrid SUV The home mortgage firm rises 3.8% in February and the average interest moderates to 3.33%
The home mortgage firm rises 3.8% in February and the average interest moderates to 3.33% This is how housing prices have changed in Spain in the last decade
This is how housing prices have changed in Spain in the last decade The home mortgage firm drops 10% in January and interest soars to 3.46%
The home mortgage firm drops 10% in January and interest soars to 3.46% The jewel of the Rocío de Nagüeles urbanization: a dream villa in Marbella
The jewel of the Rocío de Nagüeles urbanization: a dream villa in Marbella Institutions: senators want to restore the accumulation of mandates and put an end to the automatic presence of ex-presidents on the Constitutional Council
Institutions: senators want to restore the accumulation of mandates and put an end to the automatic presence of ex-presidents on the Constitutional Council Europeans: David Lisnard expresses his “essential and vital” support for François-Xavier Bellamy
Europeans: David Lisnard expresses his “essential and vital” support for François-Xavier Bellamy Facing Jordan Bardella, the popularity match turns to Gabriel Attal’s advantage
Facing Jordan Bardella, the popularity match turns to Gabriel Attal’s advantage Europeans: a senior official on the National Rally list
Europeans: a senior official on the National Rally list These French cities that will boycott the World Cup in Qatar
These French cities that will boycott the World Cup in Qatar Football: mysterious serial attacks on footballers in Malaysia
Football: mysterious serial attacks on footballers in Malaysia Paris 2024 Olympic Games: “a shame”, “level 0 of music”… The choice of JUL deeply regretted on social networks
Paris 2024 Olympic Games: “a shame”, “level 0 of music”… The choice of JUL deeply regretted on social networks Real Madrid-Bayern Munich: “I feel bad”, Manuel Neuer a fallen hero
Real Madrid-Bayern Munich: “I feel bad”, Manuel Neuer a fallen hero Mercato: Nacho should leave Real Madrid at the end of the season
Mercato: Nacho should leave Real Madrid at the end of the season