It is a cry of alarm launched by the French Society of Neonatology: while neonatal mortality has been increasing for ten years in France, the number of intensive care beds to care for the most fragile babies is “insufficient and unevenly distributed across the territory,” explains the learned society in a report published Monday.
Experts have conducted several surveys since the end of 2021, exploring the provision of care (in neonatology and critical care) and the quality of life at work of the professionals who work there. And they consider the results “very worrying”. The number of neonatal intensive care beds, already insufficient, is being reduced due to closures linked to lack of staff while more and more premature babies are taken care of and the rate of pregnancies continued despite a serious fetal malformation is also increasing. in (200% in ten years, according to the Biomedicine Agency). The beds are also very unevenly distributed across the territories: it varies “from single to double” depending on the region (from 0.6 to 1.28 beds per 1000 births, and from 0.96 to 2.84 overseas) . The worst-off metropolitan region is Provence-Alpes-Côte-d’Azur, and the southern half of the country is generally worse off than the northern half.
» READ ALSO - How to improve the care of premature babies
Consequence: “Occupancy rates are very high”, generally above 90%, or even 100% “around 20% of the time”. However, “high occupancy rates are associated with an increase in the risk of severe morbidity and mortality in very premature babies,” warns the learned society. During a survey conducted in February 2023, 23% of the services questioned said they “regularly refuse critical entries due to lack of space”. It has become common during bronchiolitis epidemics to see the alert level exceeded and babies being hospitalized very far from home, due to lack of space where they were born. This was particularly true during the winter of 2022-2023.
As everywhere in hospitals, caregivers suffer from a degraded quality of life at work and a shortage of staff. 80% of the services surveyed are struggling to fulfill their on-call schedules, and “at least one pediatric neonatologist position is vacant in 73% of type 3 services” i.e. those authorized to receive the most vulnerable newborns. at risk. 80% of the 721 pediatric neonatologists who responded said they worked more than 50 hours per week, and 13% more than 75 hours! An exhausting pace of work, which pushes some to consider giving up. The situation is no better for nurses: in eight out of ten departments, at least a third of the workforce has less than 2 years of experience, even though this is the duration considered necessary to be fully competent in these areas. very special services. But they struggle to retain their staff. And the numbers remain insufficient: the ratio between actual nursing numbers and desirable theoretical numbers is less than 1 between 60 and 70% of days, depending on the criteria used.
This sad observation is made while the infant mortality figures are not good and are deteriorating in France, experts point out: since 2012, the number of neonatal deaths has been increasing and higher than the European average since 2015. “With a excess of around 1,200 deaths each year, France, which was in 3rd position among the countries with the lowest infant mortality in Europe between 1996 and 2000, is now in 20th position,” they write, citing statistics from INSEE, INED and Europeristat. First victims: infants less than one month old (74% of deaths, compared to 65% in 2005). Various hypotheses are put forward to explain these poor results, starting with the increase in risk factors (age of the mother, increase in multiple pregnancies, precariousness, etc.). Conversely, the good results of the Nordic countries, which are distinguished by a very low stillbirth rate (2.2 to 2.5 deaths per 1000 births in 2019 for Denmark, Finland and Norway, compared to 3.6 in France ) could be explained in particular by better “inclusion of parents as care partners” (hospitalization in family rooms, developmental care programs centered on the child and family, etc.).
 Taliban, Putin, Netanyahu: the imposing hunt of Karim Khan, ICC prosecutor
Taliban, Putin, Netanyahu: the imposing hunt of Karim Khan, ICC prosecutor War in Ukraine: without Russia, Crimea will become “one of the best places to live in Europe”, assures Zelensky
War in Ukraine: without Russia, Crimea will become “one of the best places to live in Europe”, assures Zelensky British justice: traditional wigs, deemed “discriminatory” by black lawyers, about to be abandoned
British justice: traditional wigs, deemed “discriminatory” by black lawyers, about to be abandoned Israel: for the first time, Eden Golan sings in public the original version of her song rejected during Eurovision
Israel: for the first time, Eden Golan sings in public the original version of her song rejected during Eurovision Cancer: Klineo, a platform allowing patients to access new therapies
Cancer: Klineo, a platform allowing patients to access new therapies Suicide attempts and self-harm on the rise among young girls
Suicide attempts and self-harm on the rise among young girls In Europe, 10,000 people die every day from cardiovascular disease
In Europe, 10,000 people die every day from cardiovascular disease Brussels raises Spanish GDP forecasts to 2.1% and foresees a deficit of 3% in 2024
Brussels raises Spanish GDP forecasts to 2.1% and foresees a deficit of 3% in 2024 One dead and 30 injured, including 6 in critical condition, after “severe turbulence” on a London-Singapore flight
One dead and 30 injured, including 6 in critical condition, after “severe turbulence” on a London-Singapore flight At home, in restaurants or in bars... Tea fills more and more French people's cups
At home, in restaurants or in bars... Tea fills more and more French people's cups France is the fourth largest tourist economy on the planet, according to the World Economic Forum index.
France is the fourth largest tourist economy on the planet, according to the World Economic Forum index. The Navigo pass is finally available on iPhone
The Navigo pass is finally available on iPhone Injured during a football match, Yannick Noah cancels his summer concerts
Injured during a football match, Yannick Noah cancels his summer concerts Mischa Aznavour: “Tahar Rahim as Charles Aznavour, it’s class!”
Mischa Aznavour: “Tahar Rahim as Charles Aznavour, it’s class!” For Charles Aznavour's 100th birthday, a plaque in Paris where the singer lived during the Second World War
For Charles Aznavour's 100th birthday, a plaque in Paris where the singer lived during the Second World War Charles Aznavour: when Universal Music enthusiasts play detective
Charles Aznavour: when Universal Music enthusiasts play detective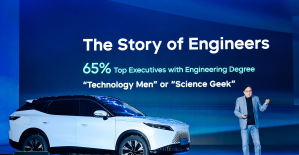 Omoda 7, another Chinese car that could be manufactured in Spain
Omoda 7, another Chinese car that could be manufactured in Spain BYD chooses CA Auto Bank as financial partner in Spain
BYD chooses CA Auto Bank as financial partner in Spain Tesla and Baidu sign key agreement to boost development of autonomous driving
Tesla and Baidu sign key agreement to boost development of autonomous driving Skoda Kodiaq 2024: a 'beast' plug-in hybrid SUV
Skoda Kodiaq 2024: a 'beast' plug-in hybrid SUV The home mortgage firm rises 3.8% in February and the average interest moderates to 3.33%
The home mortgage firm rises 3.8% in February and the average interest moderates to 3.33%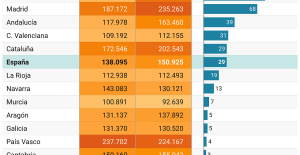 This is how housing prices have changed in Spain in the last decade
This is how housing prices have changed in Spain in the last decade The home mortgage firm drops 10% in January and interest soars to 3.46%
The home mortgage firm drops 10% in January and interest soars to 3.46% The jewel of the Rocío de Nagüeles urbanization: a dream villa in Marbella
The jewel of the Rocío de Nagüeles urbanization: a dream villa in Marbella At the Lutte Ouvrière festival, the dreams of Trotskyist revolution collide with the reality of the European elections
At the Lutte Ouvrière festival, the dreams of Trotskyist revolution collide with the reality of the European elections “Such a dear friend on whom I could always count”: the political class pays tribute to the former mayor of Marseille, Jean-Claude Gaudin
“Such a dear friend on whom I could always count”: the political class pays tribute to the former mayor of Marseille, Jean-Claude Gaudin New Caledonia: Valls pleads for a “global agreement”, Knafo judges that “France must stick to its positions”
New Caledonia: Valls pleads for a “global agreement”, Knafo judges that “France must stick to its positions” New Caledonia: Braun-Pivet wants a postponement of the Congress
New Caledonia: Braun-Pivet wants a postponement of the Congress These French cities that will boycott the World Cup in Qatar
These French cities that will boycott the World Cup in Qatar Paris 2024 Olympics: injured, Australian football star Sam Kerr will not participate in the Games
Paris 2024 Olympics: injured, Australian football star Sam Kerr will not participate in the Games Tour of Italy: Pogacar knocks out the Giro a little more... despite Alaphilippe's new number
Tour of Italy: Pogacar knocks out the Giro a little more... despite Alaphilippe's new number Volleyball: great start for Blues in the League of Nations
Volleyball: great start for Blues in the League of Nations Tennis: Gaston passes the first round in Lyon, Müller stopped by Kotov
Tennis: Gaston passes the first round in Lyon, Müller stopped by Kotov